Luteal phase management during assisted reproduction is increasingly pursued for its potential to contribute to positive reproductive outcomes.
Luteal phase support is usually performed with progesterone (P), either natural (more frequently used) or synthetic; and different routes of progesterone administration are used.
The type, doses and routes of progesterone vary among the different clinicians and centers. Given the different ways of administering progesterone, the luteal phase has not been routinely monitored. To monitor the luteal phase, serum P seems to be the best biomarker, in order to ensure that the absorption of P is adequate.Nevertheless, this was not used because serum and uterine progesterone levels are not directly correlated, and, supposedly, uterine levels were more important. On the other hand, variations of serum P levels occur in natural and stimulated cycles (depending on the pulsatile secretion from corpus luteum) and when parenteral exogenous P is given.
On the contrary, in artificial cycles and when using vaginal progesterone, steady levels of P are present after 6 hours from the onset of progesterone administration, which facilitates the measurement of the serum P levels in this scenario.
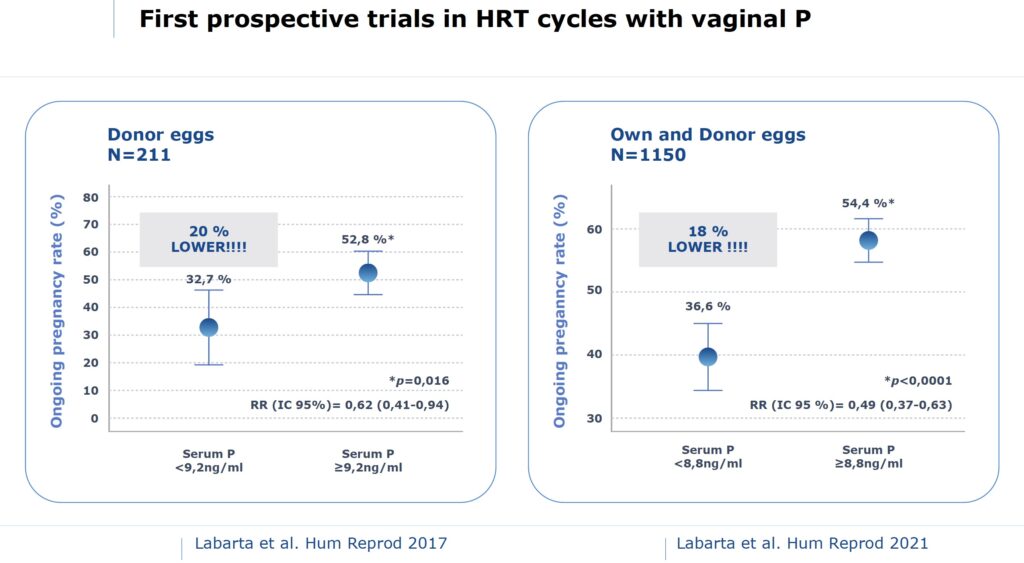
Surprisingly, recent publications indicate that serum P levels in the mid luteal phase are associated with the chances of pregnancy after embryo transfer. Data from clinical trials including almost 1400 patients suggest that the critical threshold of serum P is around 9 ng/mL. Patients who exhibited lower levels showed a significantly lower ongoing pregnancy rate and higher miscarriage rate. These findings,combined with retrospective data, suggest that a minimum level of serum P is required to optimize clinical outcome.
Notably, these results can be extrapolated only to artificial cycles and, most importantly, use of vaginal natural-like progesterone, as preferred by many clinicians worldwide. Other studies suggest that this effect is also present when using other routes of P administration and other types of cycle (e.g, natural or stimulated IVf cycle).
The need to measure serum P is now apparent, but many questions remain. More research is needed to establish which is the best dose for each patient, according to the type of cycle, route of administration and individual characteristics.
According to our results, one out of three patients receiving vaginal P showed inadequate levels of serum P, and this led to an 18% lower ongoing pregnancy rate. On the other hand, there are some variables influencing the serum P levels, i.e., weight decreases serum P levels or even the time frame between the last dose of P and the time of measurement. This has to be taken into account when interpreting the results.
According to the clinical data available, it is time to measure serum P levels and adapt the dose or the route according to the needs of the patient.
According to our experience, this adjustment proves effective. In fact, we have recently shown that addition of subcutaneous P when serum P levels were low, improves the chances of pregnancy (under review). Patients with low serum P levels on the day of ET, received an extra dose of subcutaneous P and the ongoing pregnancy was absolutely comparable to those with normal serum P levels.
Fortunately, we have begun to find a solution to the problem which has been identified.
Thus, the era of individual luteal phase supplementation (iLPS) has begun.





