When Drs. Robert G. Edwards and Patrick Steptoe successfully fertilized a human egg, grew it briefly in a petri dish, and transferred it into a woman’s uterus to produce a baby, a new era in medicine was begun [1]. This groundbreaking achievement enabled millions of infertile couples to conceive. Consequently, in 2010 Dr. Edwards was awarded the Nobel Prize for physiology/medicine, while Dr. Steptoe, who died in 1988, could not share the award as Nobel prizes are not awarded posthumously.
Not unlike many other pioneers of science, Edwards and Steptoe achieved what they did despite a skeptical establishment and many vocal critics, some of whom believed that the idea of a “test tube baby” was immoral. They could not obtain funding from the government and they had to rely on private sources to conduct their experiments in the small hospital laboratory outside Manchester, United Kingdom, where they delivered the world’s first IVF baby, Louise Brown, on July 25, 1978.
Soon after the first IVF birth came the concepts of controlled ovarian hyperstimulation to generate more than one egg per cycle [2], followed by embryo [3] and oocyte [4] cryopreservation, pre-implantation genetic testing for monogenic disorders (PGT-M) [5,6], and intracytoplasmic sperm injection (ICSI) to overcome fertilization defects [7]. As it was the case for Drs. Edwards and Steptoe, many of the researchers who contributed to these advances in assisted reproductive technologies (ART) relied on private financing and faced heavy criticism from conservative opinion-makers.
Today, encouraged by the rapid advances in the field of assisted reproduction that took place in the past four decades, we dare to predict that the field will continue to evolve, and evolve rapidly. The key questions are: where to go from here and how to pay for the journey? In our attempt to identify worthy targets for future research, we feel the need to revisit our basic mission: to achieve a healthy birth for our patients. Now we know that this can best be accomplished by elective single embryo transfer, therefore urging us to develop approaches that will allow better selection of viable embryos in the setting of ART.
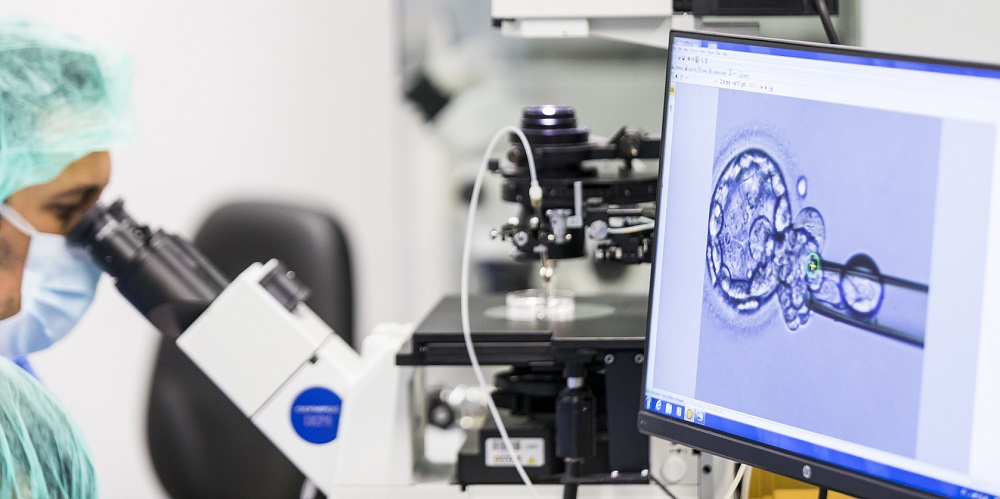
Identifying the viable embryo(s) within the cohort of embryos generated through IVF in a given cycle has long been a research focus for clinicians and embryologists.
Within this context, embryo grading systems based on cleavage rate and morphology were developed and remain the mainstay of embryo assessment and selection in the IVF laboratory [8]. Pre-implantation genetic testing for aneuploidy (PGT-A) [9], transcriptomic analysis of cumulus/granulosa cells [10], and metabolic/metabolomic analysis of spent embryo culture medium [11, 12] have been investigated as potential predictors of embryo viability. However, with the exception of PGT-A [13, 14, 15], these novel technologies have not been proven to be effective in the clinical IVF setting [10, 16-19]. Importantly, despite these advances, and under the best circumstances combining extended culture, PGT-A, and frozen embryo transfer, one third of embryos fail to implant [14]. Therefore, looking for additional biomarkers of embryo viability, whether invasive or non-invasive, seems like a worthy endeavor.
More daring research avenues, many of which are pursued at IVIRMA, include editing the embryonic genome to correct known mutations [20, 21], and introducing donor mitochondria into oocytes to prevent devastating mitochondrial diseases [22]. Particularly interesting are research aimed at allowing older reproductive age women who cannot conceive with current technologies to achieve parenthood by providing cytoplasm from younger oocytes [23], or thorough interventions that rejuvenate aging ovaries [24, 25, 26],
As important as deciding which research question to pursue is how to fund the research project and how to establish the logistics. Indeed, federal funding is often associated with a number of limitations. As an example, in the USA, yearly federal funding for infertility research is approximately 60 million US dollars. While this seems like a large number, when indirect costs (paid to academic institutions), and investigator and trainee salaries are removed, the remaining funding for actual experiments (based on our calculations) is less than 15 million US dollars per year. What is more, investigators are not allowed to experiment on embryos or even oocytes that interacted with sperm, limiting the potential for discoveries relevant to human assisted reproduction. This is where organizations like IVIRMA that are committed to scientific research and willing to channel resources to scientific discovery come into play.
We hope and believe that a collaborative effort between private organizations such as IVIRMA, federal funding agencies such as the National Institute of Child Health and Development (NICHD), and professional societies (such as the American Society for Reproductive Medicine (ASRM) and the European Society for Human Reproduction and Embryology (ESHRE)) will enable us to reach our ambitious goal of enabling each one of our patients reach their dream of parenthood.
Post by Emre Seli, M.D.
References
1-Steptoe, P. C. and R. G. Edwards. Birth after the reimplantation of a human embryo. Lancet 2: 366, 1978.
2- Trounson, A., Leeton, J., Wood, C., Webb, J., Wood, J. Pregnancies in humans by fertilization in vitro and embryo transfer in the controlled ovulatory cycle. Science 216: 681-682, 1981.
3- Trounson, A. and L. Mohr. Human pregnancy following cryopreservation, thawing and transfer of an eight-cell embryo. Nature 305: 707-709, 1983.
4- Chen, C. Pregnancy after human oocyte cryopreservation. Lancet 1: 884-886, 1986.
5- Handyside, A.H., Kontogianni, E.H., Hardy, K., Winston, R.M. Pregnancies from biopsied human preimplantation embryos sexed by Y-specific DNA amplification. Nature 344:768-70, 1990.
6- Handyside, A.H., Lesko, J.G., Tarín, J.J., Winston, R.M., Hughes, M.R. Birth of a normal girl after in vitro fertilization and preimplantation diagnostic testing for cystic fibrosis. N Engl J Med 327:905-9, 1992.
7- Palermo, G., Joris, H., Devroey, P., Van Steirteghem, A.C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 340: 17-18, 1992.
8- Gardner DK and Schoolcraft WB, In vitro culture of human blastocysts., in Towards Reprodcutive Certainty: Fertility and Genetics Beyond, M.D. Jansen R, Editor. Carnforth: Parthenon publishing. p. 378-88, 1999.
9- Scott RT Jr, Ferry K, Su J, Tao X, Scott K, Treff NR. Comprehensive chromosome screening is highly predictive of the reproductive potential of human embryos: a prospective, blinded, nonselection study. Fertil Steril, 97:870-5, 2012.
10-Uyar A, Torrealday S, and Seli E, Cumulus and granulosa cell markers of oocyte and embryo quality. Fertil Steril; 99: 979-97, 2013.
11- Seli E, Sakkas D, Scott R, Kwok SC, Rosendahl SM, Burns DH. Noninvasive metabolomic profiling of embryo culture media using Raman and near-infrared spectroscopy correlates with reproductive potential of embryos in women undergoing in vitro fertilization. Fertil Steril. 2007 Nov;88(5):1350-7.
12- Seli E, Robert C, and Sirard MA, OMICS in assisted reproduction: possibilities and pitfalls. Mol Hum Reprod 2010; 16: 513-30.
13- Scott RTJ, Upham KM, Forman EJ, Hong KH, Scott KL, Taylor D, Tao X, Treff NR. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril 2013; 100: 697-703.
14- Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, Treff NR, Scott RT Jr. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril, 100:100-7, 2013.
15- Yang Z, Liu J, Collins GS, Salem SA, Liu X, Lyle SS, Peck AC, Sills ES, Salem RD. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet, 5:24, 2012.
16- Green KA, Franasiak JM, Werner MD, Tao X, Landis JN, Scott RT Jr, Treff NR. Cumulus cell transcriptome profiling is not predictive of live birth after in vitro fertilization: a paired analysis of euploid sibling blastocysts. Fertil Steril 2018;109:460-466.
17- Vergouw CG, Kieslinger DC, Kostelijk EH, et al., Day 3 embryo selection by metabolomic profiling of culture medium with Near Infrared Spectroscopy as an adjunct to morphology: a randomized controlled trial. Hum Reprod 2012.
18- Hardarson T, Ahlstrom A, Rogberg L, et al., Non-invasive metabolomic profiling of Day 2 and 5 embryo culture medium: A prospective randomized trial. . Hum Reprod 2012; 27: 89-96.
19- Uyar A and Seli E, Metabolomic assessment of embryo viability. Semin Reprod Med 2014; 32: 141-152.
20- Ma H, Marti-Gutierrez N, Park SW, Wu J, Lee Y, Suzuki K, Koski A, Ji D, Hayama T, Ahmed R, Darby H, Van Dyken C, Li Y, Kang E, Park AR, Kim D, Kim ST, Gong J, Gu Y, Xu X, Battaglia D, Krieg SA, Lee DM, Wu DH, Wolf DP, Heitner SB, Belmonte JCI, Amato P, Kim JS, Kaul S, Mitalipov S. Correction of a pathogenic gene mutation in human embryos. Nature, 548:413-419, 2017.
21- Fogarty NME, McCarthy A, Snijders KE, Powell BE, Kubikova N, Blakeley P, Lea R, Elder K, Wamaitha SE, Kim D, Maciulyte V, Kleinjung J, Kim JS, Wells D, Vallier L, Bertero A, Turner JMA, Niakan KK. Genome editing reveals a role for OCT4 in human embryogenesis. Nature. 2017 Oct 5;550(7674):67-73.
22- Kang E, Wu J, Gutierrez NM, Koski A, Tippner-Hedges R, Agaronyan K, Platero-Luengo A, Martinez-Redondo P, Ma H, Lee Y, Hayama T, Van Dyken C, Wang X, Luo S, Ahmed R, Li Y, Ji D, Kayali R, Cinnioglu C, Olson S, Jensen J, Battaglia D, Lee D, Wu D, Huang T, Wolf DP, Temiakov D, Belmonte JC, Amato P, Mitalipov S. Mitochondrial replacement in human oocytes carrying pathogenic mitochondrial DNA mutations. Nature, 540:270-275, 2016.
23-Cohen J, Scott R, Schimmel T, Levron J, Willadsen S. Birth of infant after transfer of anucleate donor oocyte cytoplasm into recipient eggs. Lancet, 350:186-7, 1997.
24-Herraiz S, Romeu M, Buigues A, Martínez S, Díaz-García C, Gómez-Seguí I, Martínez J, Pellicer N, Pellicer A. Autologous stem cell ovarian transplantation to increase reproductive potential in patients who are poor responders. Fertil Steril, 110:496-505, 2018.
25-Herraiz S, Buigues A, Díaz-García C, Romeu M, Martínez S, Gómez-Seguí I, Simón C, Hsueh AJ, Pellicer A. Fertility rescue and ovarian follicle growth promotion by bone marrow stem cell infusion. Fertil Steril, 109:908-918, 2018.
26-Labarta E, de Los Santos MJ, Herraiz S, Escribá MJ, Marzal A, Buigues A, Pellicer A. Autologous mitochondrial transfer as a complementary technique to intracytoplasmic sperm injection to improve embryo quality in patients undergoing in vitro fertilization-a randomized pilot study. Fertil Steril, 111:86-96, 2019.